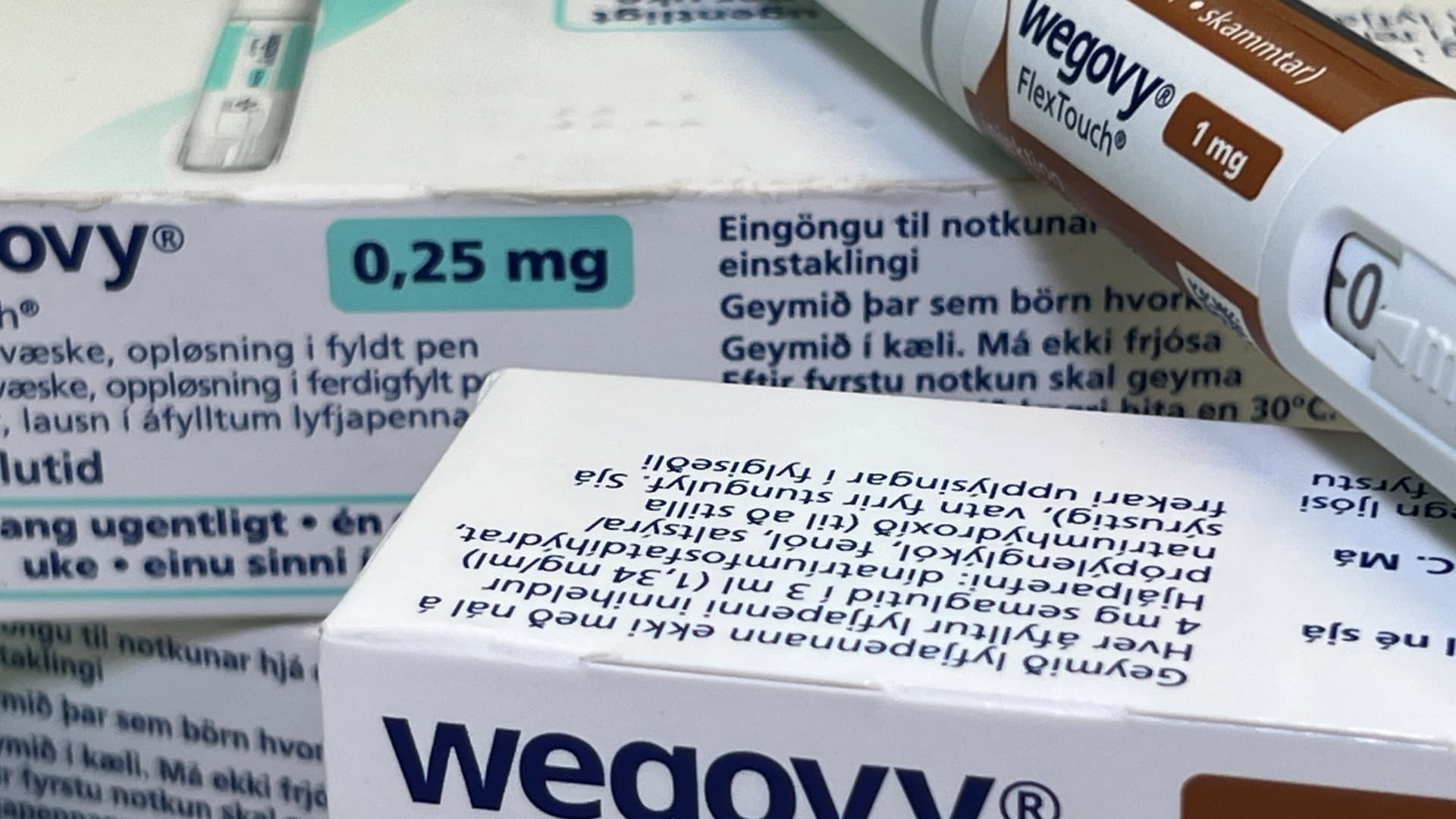
Wegovy, a popular weight loss drug in the U.S., has now been approved for heart health as well, marking a significant development in the treatment landscape. However, despite this expanded approval, insurance coverage for Wegovy and similar obesity treatments remains a contentious issue.
Many employers and health plans are hesitant to cover Wegovy due to its steep monthly price tag of $1,350, which they fear could strain their budgets. Questions also linger about the long-term effectiveness of the treatment and whether patients will stay on it indefinitely.
Insurance industry experts suggest that some plans may reconsider covering Wegovy in the future, especially as they update their formularies. However, the road to broader coverage for weight loss drugs may be fraught with challenges, as insurers grapple with the cost implications and potential impact on overall healthcare spending.
Advocates for broader coverage of weight loss drugs argue that these treatments could yield long-term cost savings and improve health outcomes for patients. The recent approval of Wegovy for its cardiovascular benefits underscores the potential downstream health effects of weight loss medications, challenging the notion that such treatments offer only cosmetic benefits.
Despite the potential benefits of covering weight loss drugs, concerns about costs and uncertainty surrounding long-term use continue to hinder widespread insurance coverage. The evolving landscape of obesity treatment underscores the need for a nuanced approach to coverage decisions, balancing financial considerations with patient care.